We are one of the only neurospine clinics that accepts Tricare and Triwest. Let us return the favor, in helping you, with a better life.

We are one of the only neurospine clinics that accepts Tricare and Triwest. Let us return the favor, in helping you, with a better life.

The ouch part of pain begins when something—heat, certain chemicals or a mechanical force—activates special nerve endings called nociceptors. Once they are activated, they trigger a cascade of events with a representation of that signal going through your nerves and into your spinal cord and then to the brain. And that’s when things get really complex.
Pain signals interact with many different brain areas, including those involved in physical sensation, thinking and emotion. That leads to all the complexities of what we feel associated that initial hurt.
Having an emotional component linked to the sensory experience is a great memory enhancer. If you touch a hot stove your brain remembers, and you will never do that again.
The link between pain and emotion is a good thing, but sometimes it can also be destructive. Mental health disorders amplify pain. They engage regions of the brain that associate with pain processing, and they can also facilitate rumination and fearful focus on the pain. And when pain doesn’t go away it can cause disabling changes in the brain. Pain is a danger signal, but once pain becomes chronic these pain signals no longer serve a useful purpose. Over time, these signals can lead to problems like depression, anxiety and stress, but it’s often possible to break that cycle by learning techniques that help pain patients gain some control of the way their brains are processing pain signals. For example, a state of relaxation is an antidote to the hard-wired pain responses that are automatically triggered by the experience of pain.
For some patient techniques like these can provide an alternative to pain drugs, including opioids. And for pain patients who rely on medications, psychological therapies can often help the drugs work better.
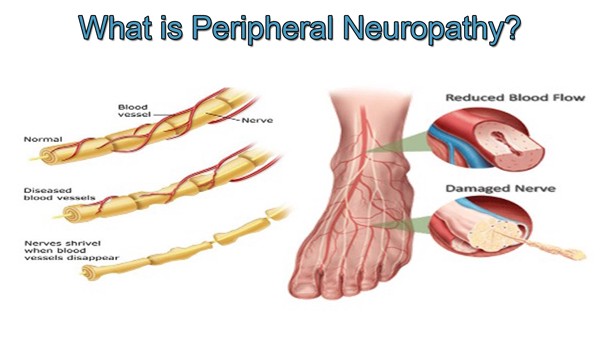
Peripheral neuropathy is a disorder caused from damage to the endings of the nerves. Patients frequently report burning, itching, or shooting pain that often begins in the feet and gradually progresses to other areas. Peripheral neuropathy is a symptom of an underlying disease or process and tested to find out the underlying cause. EMG and nerve conduction testing performed by a trained physician can help rule out other causes of these symptoms and help plan for the best course of treatment. Our neurologists are trained in advanced EMG and nerve conduction testing and are well-versed in diagnosing and managing peripheral neuropathy.

“What can I do to reduce my chance of Alzheimer’s?” As a neurologist, this is one of the most common questions I am asked. My reply was typically “select different parents, get better genes” as little was known beyond that as far as a risk factors for many diseases of the nervous system. We still do not know exactly why people get ALS, Parkinson’s disease, amongst others, but it seems to be more and more clear that while nutrition is not the only factor, it is an extremely important one. More and more studies are being completed that show healthy people get less chronic disease including diseases of the nervous system. There is an abundance of information that comes at us from all directions which can be conflicting and confusing. I have now discovered a resource that I feel confident enough to guide my own and my family’s nutrition and a resource I refer patients to.
Nutritionfacts.org is a nonprofit organization founded by Michael Greger, MD, FACLM to provide science behind nutrition recommendations. He has videos discussing the science behind ketogenetic diets, artificial sweeteners, which plans to eat to combat certain diseases, amongst 100s of other topics. And, it is an invaluable FREE resource. Of note, I have no relationship with this site nor Dr Greger. I am just a very happy recipient of the information given by his nonprofit organization.
If a more healthy diet seems out of reach financially, here are a few additional resources to consider:
Based in Michigan, this initiative has a national Double Up Food Bucks program that doubles the value of federal Supplemental Nutrition Assistance Program (SNAP, or food stamps) benefits at farmers’ markets and grocery stores.
This Detroit-based program caters to low-income patients with chronic diseases, caregivers of young children, and pregnant women who are referred by their primary care physicians. Patients receive a prescription for produce that’s filled at partnering farm stands or markets.
This national organization can help people start a produce prescription program in their own area. Contact them for a tool kit that includes fundraising strategies and step-by-step instructions.
” Do you know a doctor who deserves recognition? We want to know who you think are the top doctors in the state.
Tell us your favorite doctor in the 25 categories below. Doctors with the most nominations will appear in our Top Doctors list in the Winter issue of Arkansas Life.
Please click on the ‘Top Doctors 2020‘ to be taken to the correct website.
https://arkansaslife.com/doctors/

Legacy Spine and Neurological Specialists proudly hosts former PGA professional and one of the top PGA instructors in the nation Stan Utley to Chenal CC in Little Rock last week. Stan presented a short game seminar to participants in the Oak Leaf Classic. Then see how I actually somehow caught on and carried out a great surgical removal of the ball from the deep rough almost holing out!
To Learn more about his short game expertise visit stanutley.com
Stan’s principles of the golf swing is to utilize the dead weight of the clubhead to do the work. Using the momentum of the dead weight of the clubhead and wrists to direct such certainly allows one to swing the clubhead faster with much less effort. Swing fast not hard he explains. Accelerate the clubhead not the grip!
Swinging hard and/or incorrect posture can lead to sports spine issues just as incorrect posture and ergonomics can lead to work and activities of daily life spine injuries. Injury prevention not only can improve your game but your life more importantly (if anything is more important than golf?)!
To learn more about how to best prepare your spine for life’s sports and daily activities or to see treatment please visit our website LegacyNeuro.com or make an appointment to see our physical therapist Jessica Beggs who has vast expertise in spine physical therapy treatment and prevention of injuries. Incidentally if you suffer from Golfer’s or Tennis’ Elbow issues reach out to Jessica as well. She has done wonders with mine!
Fall, A Season? Or a Safety Concern?

With the leaves changing and seasons turning it is time to talk about “Fall”, but perhaps not in the way you are thinking. As the weather changes and the temperature outdoors starts to decrease the incidence of fall related injuries has been noted to increased1. A good working definition for the context of fall that we will be discussing is any event that leads to an unplanned, unexpected contact with a supporting surface2 . Here at Legacy we have an interconnected team of specialists that can identify risk factors that may predispose a patient for falls then provide timely intervention and recommendations on how to decrease the risk of falling.
A few quick statistics to emphasize the importance of intervention in patients with poor balance:
If you are feeling unsteady on your feet, constantly worrying that a fall is imminent, or pain has started limiting your mobility then reach out to your local medical doctor, someone from the Legacy Team, or your local physical therapist for a treatment plan that will have you ready for Spring!
1 Pui-Yee, et al. Higher incidence of falls in winter among older people in Hong Kong.
2 Tinetti ME, Ginter SF. Identifying mobility dysfunctions in elderly patients: standard neuromuscular examination or direct assessment? JAMA. 1988;259:1190-1193.
3 Tinetti ME, Speechley M Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1989:319: 1701-1707.
4 Nevitt MC, Cummings SR. Risk factors for recurrent non-syncopal falls: a prospective study. JAMA. 1989;261:266.7-2668.
5 Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-dwelling elders. J Gerontology. 1994;49:M140-M147.

Cervicogenic headaches are an often-overlooked headache type. These headaches cause pain in the back of the head, the temporal areas, and behind the eyes and are often mistaken for—or co-exist with—tension headaches, migraine headaches and neck pain. Often patients with cervicogenic headaches will have a history of a neck injury such as whiplash, or participate in activities that cause excess stress to the upper neck such as working on computers or looking down at smart phones. Poor posture is also a factor.
The treatment for this type of headache starts with physical therapy which helps most people. Sometimes medications like muscle relaxers, gabapentin or Lyrica are used to help treat the pain. For people whose headaches are refractory to conservative treatments, procedures like occipital nerve blocks, steroid injections or percutaneous radiofrequency neurotomy can provide lasting relief.
Many migraine patients recognize specific triggers to their headaches. Migraine patients are more sensitive to certain substances in their foods and environments as well as changes to their routine. Too much or too little sleep, changes in exercise routines, and processed foods can worsen migraine headaches. Heavy, flowery scents or cigarette smoke are frequent triggers. Keeping a headache journal can help identify migraine triggers and eliminate them. Elimination diets that target artificial sweeteners, food dyes, chocolate, processed meats, and/or certain alcohols can help find food triggers. In general, migraine patients are encouraged to eat a diet consisting of whole foods, stay hydrated, avoid caffeine, have a regular sleep schedule, and exercise regularly.

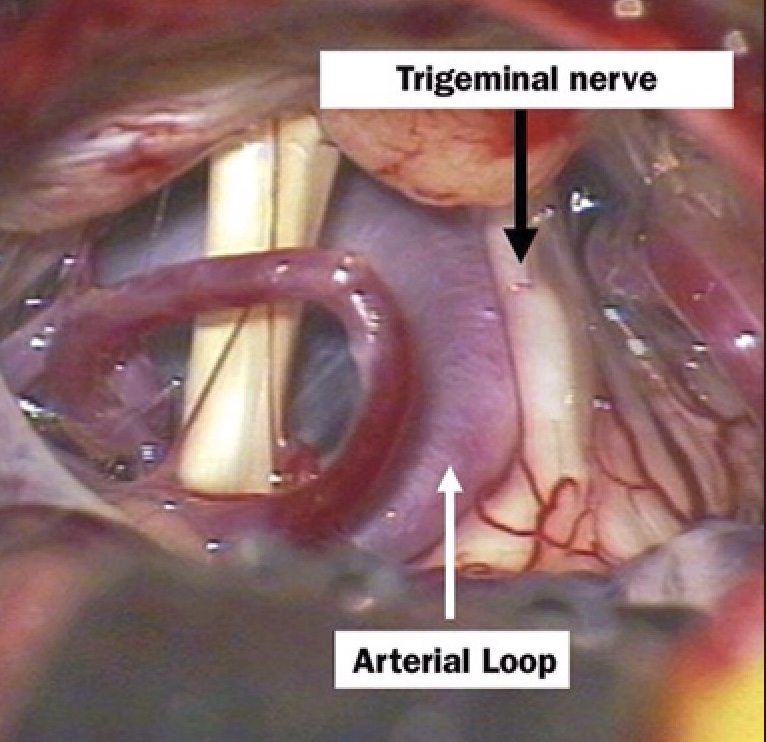
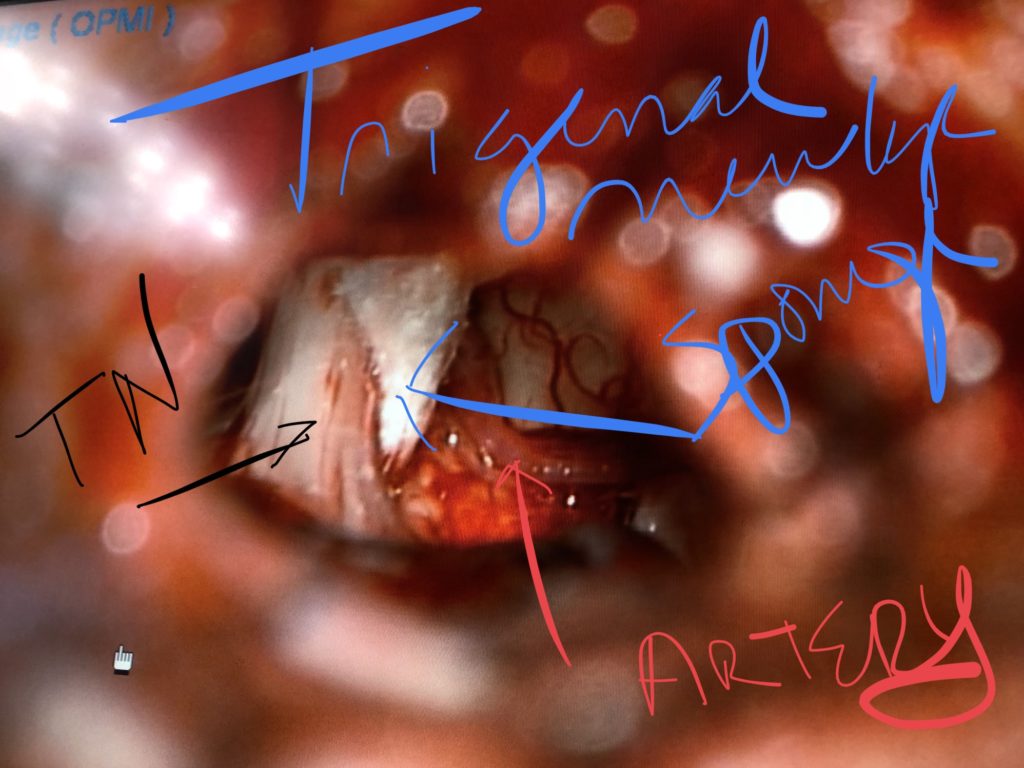
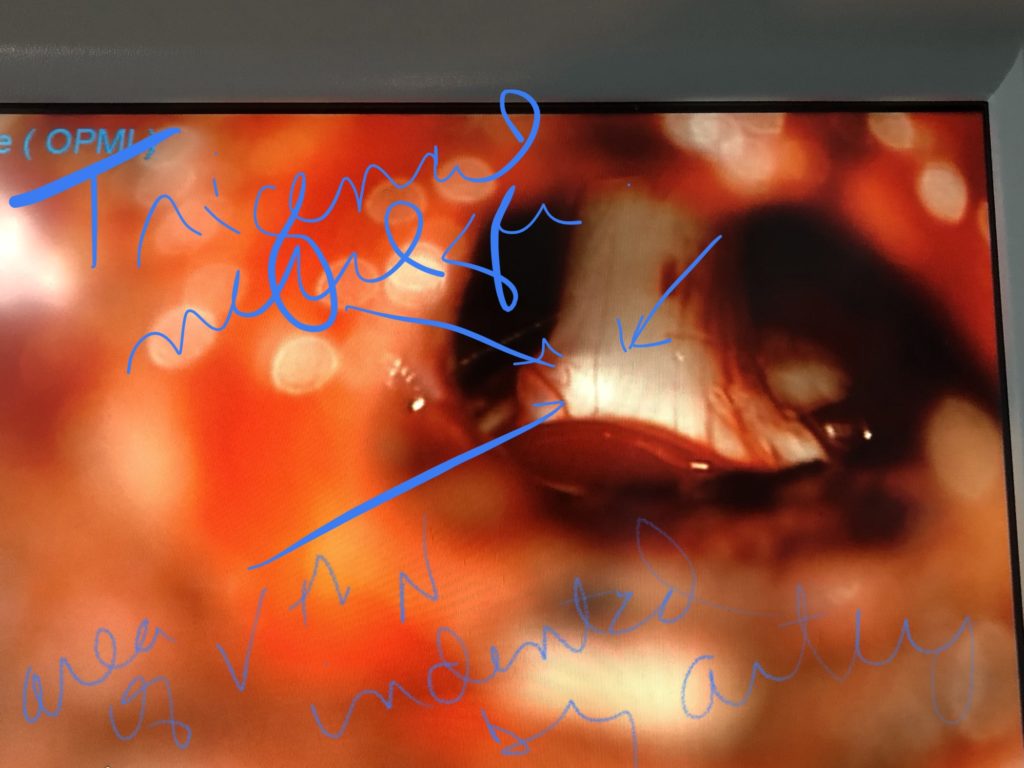
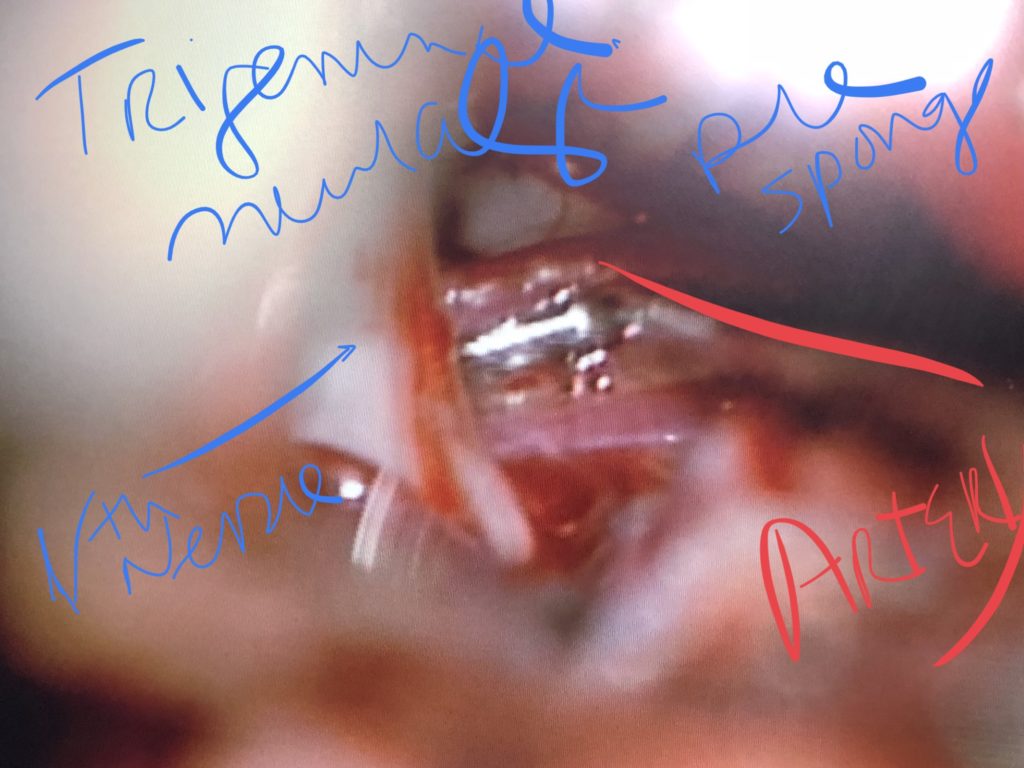
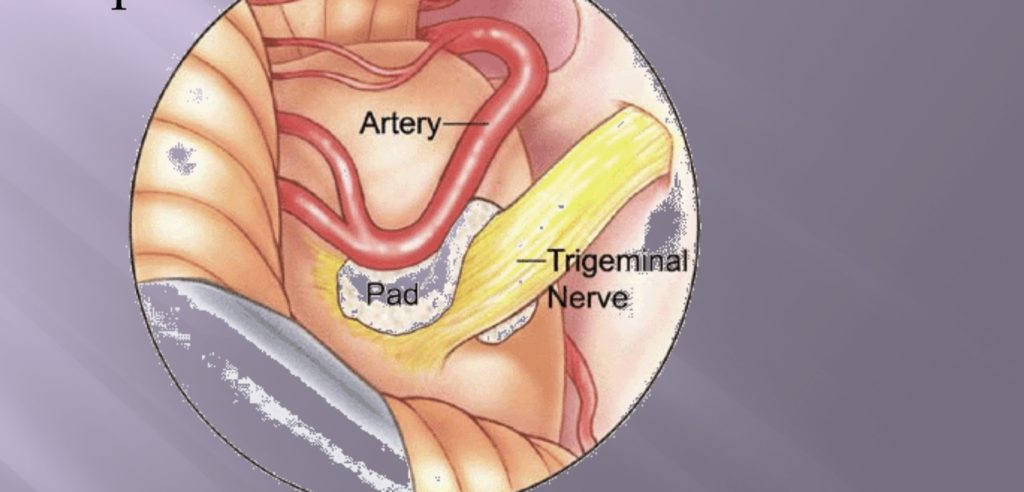
Trigeminal Neuralgia is a facial pain disorder caused by compression of the 5th Cranial nerve deep in the brain by an adjacent artery. This condition, also know as Tic douloureux or “Suicide disease” is often misdiagnosed and mistreated. It is the most painful neurological disorder that exists. The disorder causes horrific electrical shocking pains on one side of the face that come and go very rapidly like a machine gun of taser strikes. If properly diagnosed it can be readily cured with a low recurrence rate and low risk of complications by experienced surgeons for those that fail medical treatment. For all, to learn more about TN please visit https://youtu.be/pOV3EC3lpJw for our educational video.